Hepatitis is a group of viral infections that cause inflammation of the liver, leading to varying degrees of liver damage and impaired liver function. Over the years, significant advancements have been made in the diagnosis, treatment, and prevention of hepatitis, resulting in improved overall health outcomes. Diagnostic tools such as blood tests and imaging techniques have enabled more accurate and timely detection of hepatitis infections, allowing for early intervention and appropriate management. Effective antiviral therapies have been developed, leading to higher rates of viral suppression and cure for certain types of hepatitis. Additionally, vaccination programs have played a crucial role in preventing hepatitis infections and reducing their burden.
Despite these advancements, hepatitis remains a significant global health problem, affecting millions of people worldwide and posing substantial challenges in terms of prevention, diagnosis, and access to treatment. On world hepatitis day, we take a look at autoimmune hepatitis (AIH), a rare but important cause of liver morbidity and mortality.
Autoimmune hepatitis
Autoimmune hepatitis refers to non-contagious, chronic and progressive inflammation of the liver which can lead to cirrhosis, acute liver failure, and other severe complications. The aetiology of AIH remains unknown, but evidence suggests a coalescence of genetic susceptibility and environmental risks, which culminate in a loss of immune tolerance leading to T-cell-mediated destruction of hepatocytes. There are two known types of autoimmune hepatitis. Type 1 is distinguished by the presence of anti-smooth muscle antibodies (ASMA) with or without anti-nuclear antibodies (ANA). Type 2 autoimmune hepatitis presents with positive anti-liver/anti-kidney microsome (anti-LMK) type 1 antibodies or anti-liver cytosol (anti-LC) type 1 antibodies.
Diagnosis of autoimmune hepatitis (AIH) is multifaceted, involving a combination of clinical, biochemical, immunological, and histological factors, whilst also excluding other liver diseases with similar features. There is no single diagnostic test for AIH, and a liver biopsy is considered mandatory in the diagnostic process. To aid in diagnosis, various diagnostic scoring systems have been developed, such as those by the International Autoimmune Hepatitis Group (IAIHG) for adult patients. These scoring systems consider both positive criteria, including autoantibodies and elevated IgG levels, and negative criteria, which exclude other liver diseases. Autoantibodies play a crucial role in AIH diagnosis and differentiation between AIH types. Specifically, ANA and SMA characterize AIH-1, while anti-LKM-1 and anti-LC-1 define AIH-2. However, some cases may present with a combination of autoantibodies. Different techniques, such as indirect immunofluorescence (IIF) or commercially available enzyme-linked immunosorbent assays (ELISAs), can be used to detect these autoantibodies. Despite advances in diagnostic scoring systems, AIH diagnosis continues to rely on a comprehensive evaluation of various factors and requires ongoing research to enhance diagnostic accuracy and clinical applicability.
The Importance of Biomarkers in AIH
In the context of AIH, ideal biomarkers should be non-invasive, easily measurable, cost-effective, and reproducible across different patient populations. They should also be sensitive enough to detect liver histologic inflammatory activity, predict remission following immune suppressive treatment (IST), and identify patients at higher risk of relapse to guide personalized therapeutic decisions. There is an urgent need for additional biomarkers for AIH to complement traditional markers and improve diagnostic accuracy and treatment monitoring.

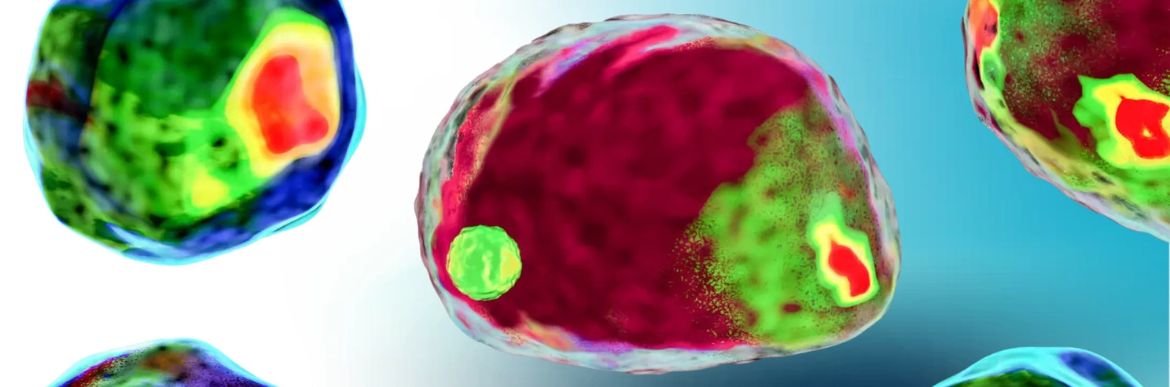
Figure 1: Depiction of the progression of autoimmune hepatitis with associated potential biomarkers of activity and quiescence at each stage of disease.
Adapted from: Hepatology76(6):1862-1879, December 2022.
Promising Candidate Biomarkers
Researchers have identified several potential candidate biomarkers that could enhance the management of AIH. These biomarkers include markers of subclinical disease activity, predictors of clinical relapse, and markers of treatment response. Some of these biomarkers have been borrowed or adapted from other immune-mediated diseases such as liver transplantation and drug-induced liver injury.
Preclinical Biomarkers
Currently, there are no known preclinical biomarkers capable of identifying signs of autoimmune hepatitis (AIH) before clinical detection or liver damage. However, certain genetic polymorphisms, such as DRB1*03:01, SH2B3, and CARD10, have been associated with AIH. These genetic markers may be helpful for risk stratification in patients with other autoimmune features who may be at a higher risk for developing AIH. However, they are fixed values and lack utility in monitoring disease progression over time.
Clinical Phase Biomarkers
During the initial presentation of AIH, specific biomarkers may be clinically useful in detecting liver inflammation before increases in traditional serological markers of liver injury. Immune markers, such as IL-17A and TNF-α, have been found to be significantly increased in AIH patients, indicating a potential trackable immune marker of disease activity. Serum adenosine deaminase (ADA) levels and TGF-ß1 have also shown correlations with the severity of interface hepatitis, making them potential biomarkers for grading disease severity at initial presentation. Additionally, serum BAFF (B-cell activating factor) levels have been found to be elevated in active AIH, reducing with corticosteroid treatment. Vitamin D receptor and vitamin D resistance have also been investigated, with low baseline serum 25(OH)D levels associated with nonresponse to treatment and liver-related mortality.
Remission Biomarkers
Remission in AIH can be categorized into biochemical remission, indicated by the normalization of AST, ALT, and IgG levels, and histological remission, characterized by the absence of inflammation, such as interface hepatitis, on liver biopsy. While biochemical remission is essential, it may not always reflect histological remission accurately, highlighting the need for non-invasive biomarkers to assess histological remission and reduce reliance on liver biopsies. Serum DNAse1, an enzyme involved in apoptotic cell degradation, has emerged as a potential protective biomarker associated with remission in AIH. Patients experiencing sustained remission have higher baseline DNAse1 levels compared to partial responders, nonresponders, and subsequent relapsers. The role of DNAse1 in autoantigen breakdown and its relationship to inflammation suggest that regulators of autoantigen breakdown may be important in determining the risk of disease activity versus remission in AIH. Ferritin levels have also been studied as a predictive biomarker of treatment response, with elevated baseline levels associated with complete biochemical remission.
Drug Withdrawal Prediction Biomarkers
This is arguably the most significant disease phase for the development of biomarkers in terms of clinical application. Studies have explored T cell phenotyping as potential biomarkers in AIH. The ratio of Treg (FOXP3) to Th17 (RORɣt) gene expression showed promise in distinguishing active AIH from quiescent disease, indicating a potential surrogate for liver biopsy and identifying patients with favourable phenotypes for IST withdrawal. Anti-programmed cell death (PD)-1 antibodies, which regulate T cell activation, have also been evaluated as potential biomarkers. Higher levels of serum anti-PD-1 antibodies were associated with acute AIH compared to remission, and their presence may predict poor treatment response and relapse, indicating a higher risk during IST withdrawal. The presence of anti-soluble liver antigen (SLA) antibodies has been linked to an increased risk of relapse after IST withdrawal, making them a potential prognostic marker for withdrawal consideration. Additionally, cytokeratin-18 death marker m65 has shown promise in predicting incomplete histological remission, guiding clinicians away from IST withdrawal or prompting the need for a liver biopsy.
Relapse Biomarkers
Early relapse detection is crucial in AIH as relapse is common both with and without IST withdrawal. Biomarkers in this phase would be valuable in identifying patients with resistant relapses who may require higher doses of IST to achieve remission. ANA and SMA, though part of the diagnostic criteria for type 1 AIH, are not disease-specific and do not correlate with AIH activity in adults. However, in pediatric populations, LKM-1 and SMA may correlate with disease activity. Anti-asialoglycoprotein receptor (ASGPR) titers have shown promise as potential biomarkers. They are elevated in active AIH and decrease in response to IST. Moreover, ASGPR titers may increase prior to the elevation of liver enzymes, indicating their potential to predict early diagnosis and relapse of AIH. Macrophage migration inhibitory factor (MIF) is a cytokine studied in other Th1-mediated autoimmune diseases. In AIH, MIF levels remain elevated despite corticosteroid therapy, and specific genetic variations in the MIF promoter correlate with steroid resistance. The ratio between the soluble MIF receptor (CD74) and MIF negatively correlates with ALT in relapsing patients, suggesting its potential as an immune disease activity biomarker and a marker of aggressive disease and steroid resistance. These biomarkers could significantly improve early relapse detection and facilitate tailored treatment strategies for AIH patients.
Advances in autoimmune hepatitis biomarkers are essential for improving the diagnosis, monitoring, and treatment outcomes this complex disease. While traditional biomarkers like liver enzymes and IgG levels remain valuable, they have limitations in predicting histologic remission and identifying patients at high risk of relapse. Ongoing research aims to identify novel biomarkers that are non-invasive, reproducible, and provide insight into the underlying immune mechanisms of AIH. The development and implementation of such biomarkers have the potential to revolutionize the management of AIH, leading to personalized therapeutic approaches and better patient outcomes.
Blog written by Dr. Caroline Beltran (PhD)
References:
- Harrington, C., et al. 2022. Noninvasive biomarkers for the diagnosis and management of autoimmune hepatitis. Hepatology 76(6):p 1862-1879, (2022). https://doi.org/10.1002/hep.32591
- Terziroli, B., et al. 2022. Autoimmmune hepatitis. Cell Mol Immunol 19, 158–176 (2022). https://doi.org/10.1038/s41423-021-00768-8
- Zheng, L., et al. 2021. Clinical characteristics and treatment outcomes of acute severe autoimmune hepatitis. BMC Gastroenterol 21, 93 (2021). https://doi.org/10.1186/s12876-021-01653-4
- Mieli-Vergani, G., et al. 2018. Autoimmune hepatitis. Nat Rev Dis Primers 4, 18017 (2018). https://doi.org/10.1038/nrdp.2018.17
- Corrigan, M., et al. 2015. Autoimmune hepatitis: an approach to disease understanding and management. British Medical Bulletin, Volume 114, Issue 1, June 2015, Pages 181–191, https://doi.org/10.1093/bmb/ldv021