The 29th of February 2024 marks the global observance of Rare Disease Day. On this leap day, we delve into Chronic Inflammatory Demyelinating Polyradiculoneuropathy (CIDP), a rare disease that is particularly debilitating for patients and explore the revolutionary new preclinical techniques that are being used to better understand the pathology and avenues for treatment.
A “rare disease” is defined by the WHO as having less than 65 cases per 100,000 people – CIDP has a prevalence of 0.7-10.3 cases per 100 000 so it certainly meets this threshold. It is characterised by demyelination of motor and sensory nerves and manifests as an onset of weakness, hypo or areflexia (impacted reflex response), numbness, tingling and sensory ataxia (loss of coordination). Up to 32% of CIDP patients are unable to walk independently and the search continues for a viable, effective treatment. Current intervention includes intravenous immunoglobulins, steroids and plasma exchange.
Although the exact stimulus which induces the disease is still unknown, the pathophysiology is characterised by autoreactive T-cells which secrete inflammatory cytokines, inducing the production of autoantibodies which recognise and attack neuronal proteins including myelin glycoproteins. This further recruits and activates the complement system which is deposited on myelin sheaths. Macrophages recognise complement receptors, inducing myelin sheath damage and phagocytosis. Further, complement components generate the membrane attack complex (MAC), causing targeted cell lysis of neuronal cells.
To best combat the disease, companies are investigating therapeutic interventions including various antibody-based therapies. To best screen them for effectiveness, these candidates will need to be assessed preclinically first. Traditionally, the experimental model of choice has been the experimental autoimmune neuritis (EAN) rat model. The pathology in the rats is induced by immunisation with peripheral nerve homogenate which initiates immune attack of peripheral nerve proteins. Perivascular (neuronal blood vessel) T-cell infiltrates appear after 10-12 days, resulting in paralysis and myelin destruction. While widely used, as with many animal models, translation and predictive capabilities of this model are limited.
There are simpler in vitro models available which rely on the culture of primary Schwann cells (SC’s), induced pluripotent stem cells (iPSC’s) or 3D culture of fibroblasts, SC’s and neuronal cells. SC cultures have been used to screen for autoreactive antibodies in patients with CIDP. Ideally, to best recapitulate the in vivo setting, SC’s need to be co-cultured with motor neurons. SC’s wrap around motor neuron axons as they differentiate and over a culture period of 3 weeks, demonstrate clear myelination. This latter aspect means that in order to properly model demyelination in CIDP, models need to include SC’s and motor neurons.
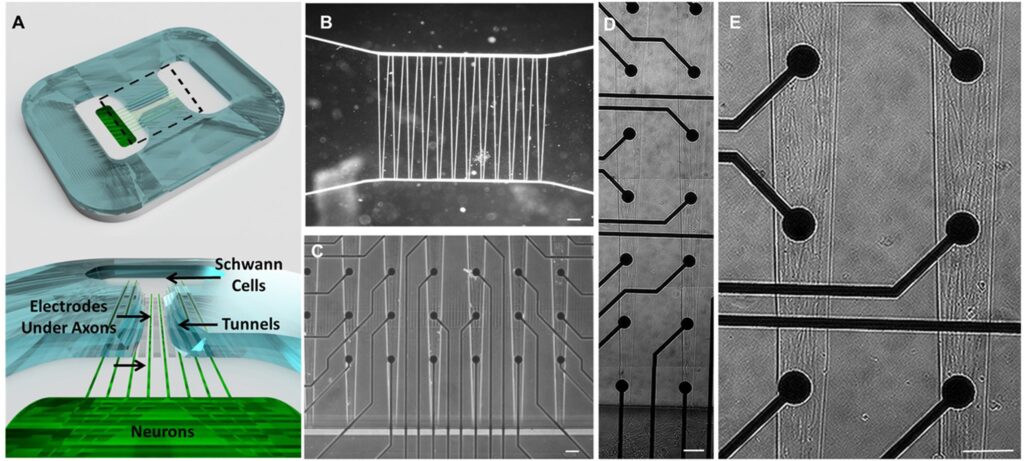
Recently, preclinical models have further expanded their complexity and include a human-on-a-chip model. This used iPSC-derived motor neurons and SC’s cultured on a microelectrode array. When treated with serum from CIDP patients, the model significantly induced the CIDP pathology including:
- Cell surface complement protein expression
- Autoantibody binding to membranes
- Complement deposition
- Blocked conduction velocity
Most critically, the pathology was rescued with an anti-complement monoclonal antibody, demonstrating how this model could successfully screen for a functionally relevant therapeutic.
At Synexa, we have had experience in profiling biomarkers and building preclinical models focused on multiple diseases including several rare conditions like CIDP. Working closely with clinicians and patient groups, we aim to build the knowledge base in these understudied areas, working with our biopharma and biotech customers to work toward effective treatments to benefit patient health.
References
- Broers et al. Neuroepidemiology. 2019;52(3-4):161-172.
- Rumsey et al. Adv Ther (Weinh). 2022 Jun;5(6):2200030