World Leprosy Day is observed on the last Sunday of January each year. Established in 1954 by French philanthropist Raoul Follereau, it aims to raise awareness about leprosy (now called Hansen’s disease) and teach people about this ancient disease that is easily curable today.
Having spent the better part of 10 years researching Tuberculosis, one cannot work on this disease and not have a deep appreciation for the exquisite pathogen that is Mycobacterium tuberculosis. Built with an elaborate and complex cell wall, M. tuberculosis has evolved numerous mechanisms that allow it to succeed as one of the deadliest pathogens in the world. But what of its cousin, Mycobacterium leprae, the causative agent of leprosy?
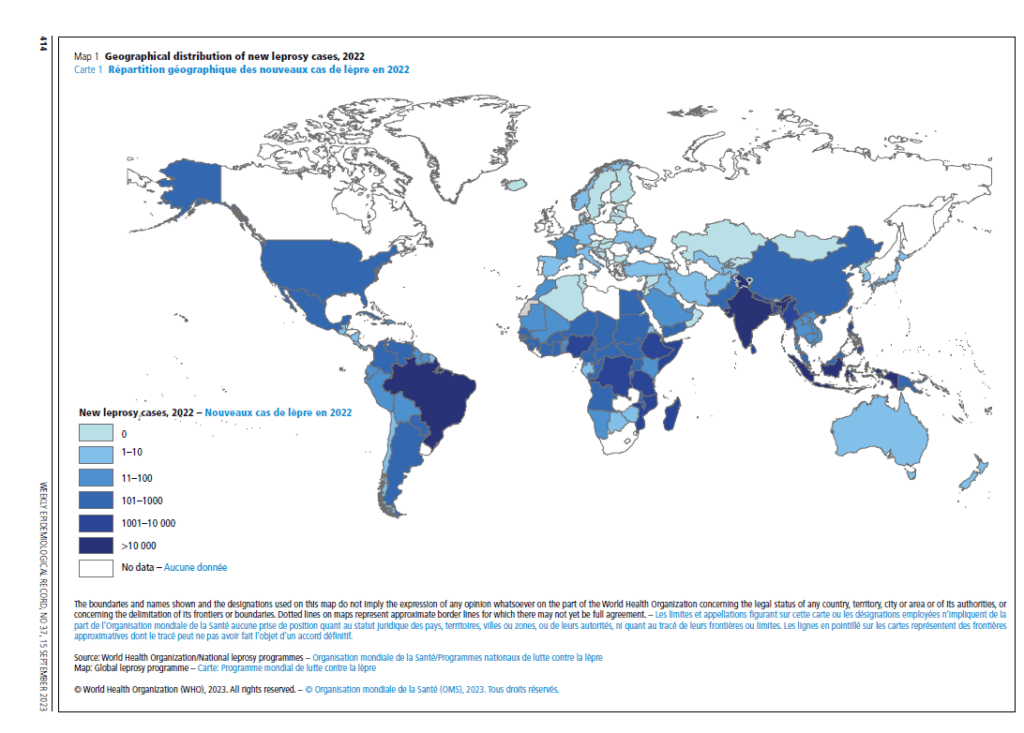
When one hears leprosy, now known as Hansen’s disease, we often think of colonies from a bygone age, an ancient disease that has surely been eradicated. The numbers are surprising. Despite the availability of drug treatment distributed free of charge by the WHO over the last 40 years, there are still more than 200,000 new cases reported every year, occurring in more than 120 countries, with close to 15,000 children diagnosed with Hansen’s disease in 2019. Despite available treatment, the disease still has a high disabling potential, particularly when diagnosed at advanced stages. It is estimated that about 25% of newly diagnosed patients each year will suffer from irreversible nerve damage and are at risk of developing classic hand or foot deformities and associated disabilities as a long-term consequence of leprosy. Approximately three million individuals around the world suffer from physical disabilities because of damage to peripheral nerves and subsequent sensorimotor loss caused by leprosy.
The challenge of studying M. leprae
Getting by with the bare minimum seems to be the modus operandi of Mycobacterium leprae and is attributed to its recalcitrance. Its genome sequence reveals that it has undergone massive genome ‘downsizing’ over time, resulting in the loss of approximately 1/3 of the coding capacity found in M. tuberculosis. Attempts to study M. leprae have been thwarted by an inability to be grown in artificial media and excruciatingly slow doubling time (once every 14 days). To circumvent this in vitro culture problem, Charles Shepard established a pioneering mouse pad infection model in the 1960s, allowing for limited multiplication of M. leprae in vivo. This model was further improved with the discovery of armadillo species as the most appropriate host species for leprosy research. Specifically, the nine-banded armadillo develops an extensive nerve involvement that closely resembles the neuropathy seen in humans.
Pathophysiology of M. leprae infection
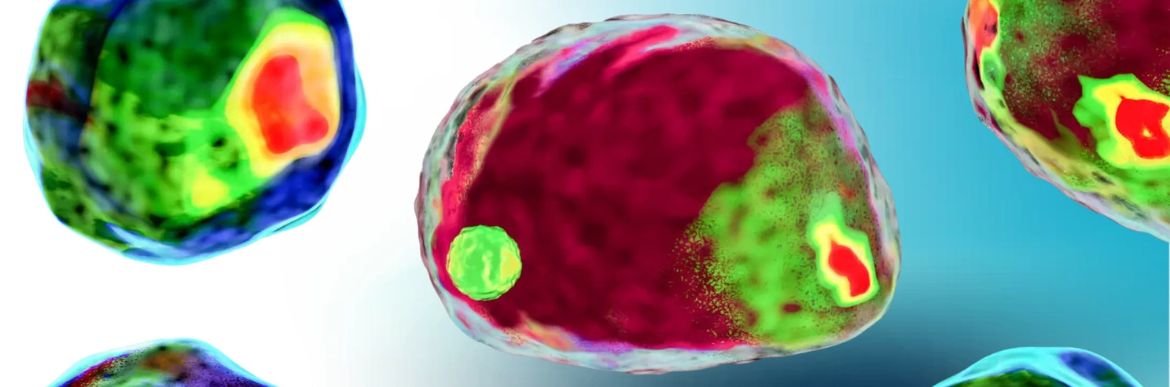
Hansen’s disease has traditionally been classified into two major types, tuberculoid and lepromatous, correlated by distinct immunological responses. The incubation period for leprosy is long, ranging from months to decades, with an estimated average time of 10 years for the lepromatous form and four years for the tuberculoid form. It is estimated that over 95% of infected individuals are naturally resistant to M. leprae, never developing any signs or symptoms of the disease. Among symptomatic individuals, after the indeterminate phase, the disease manifests itself along a horizontal spectrum, based on clinical, bacilloscopic, and histopathological characteristics, containing the two polar forms (tuberculoid and lepromatous) and three intermediate forms (borderline-tuberculoid, borderline-borderline, and borderline-lepromatous). As the clinical presentation progresses from the tuberculoid to the lepromatous pole, a gradual transition occurs from the Th1 to Th2 immune response. A key to the success of M. leprae as a persistent, obligate intracellular pathogen is its ability to survive and grow for extended periods within professional phagocytes, primarily macrophages, and Schwann cells.
Biomarker research for leprosy
The clinical diagnosis of leprosy is dependent on the recognition of disease signs and symptoms and is therefore only possible once the disease has manifested. Skin lesions are usually the first clinical manifestation observed. If appropriate medical treatment is not received, leprosy may progress to cause permanent damage to the skin, nerves, limbs, and other organs. The main diagnostic criteria include (1) a hypopigmented or erythematous skin lesion or reddish skin patch with definite loss of sensation; (2) a thickened or enlarged peripheral nerve with loss of sensation and/or weakness of muscle supplied by the nerve; and (3) a positive acid-fast skin smear or bacilli observed in a skin smear/biopsy. When all three signs were present, diagnostic accuracy was as high as 95%. Physical examination does not identify the early stages of the disease, especially when clinical manifestations are rare and it is likely that clinical diagnosis is delayed or even missed, especially in regions where leprosy is controlled. Consistent with the characteristics of a neglected disease, there are no sensitive and specific methods capable of assisting in the diagnosis of patients with early leprosy.
Efforts have been deployed to improve leprosy diagnostics using cutting-edge technologies, such as molecular identification of M. leprae, serological tests for specific bacterial antigens, and quantification of host biomarkers in plasma or in vitro whole blood assays (WBA). Currently, some specific antibodies against M. leprae have been studied as diagnostic markers, with special attention to phenolic glycolipid 1 (PGL-1). Multibacillary patients are almost all universally positive for anti-PGL-I by ELISA whereas positivity for paucibacillary patients is low, usually in the range of 20-40%. Identification of M. leprae DNA using qPCR has allowed greater sensitivity in identifying leprosy patients with inconclusive histopathological results, and head-to-head comparison with droplet digital PCR has shown even greater sensitivity and specificity for paucibacillary leprosy. More recently, bulk RNA seq was employed to compare the transcriptomes in skin lesions of leprosy patients or controls affected by other dermal conditions such as granuloma annulare, a confounder for paucibacillary leprosy. A five-gene signature was presented, capable of accurately distinguishing multibacillary and paucibacillary leprosy from other skin conditions.
Concluding remarks
Despite its ancient roots, Hansen’s disease persists in the modern era as a neglected disease, with active cases cropping up across the world. Lack of awareness remains pervasive, leading to underdiagnosis and delayed treatment. The enduring stigma surrounding this disease, as well as misconceptions around treatment, perpetuates harmful stereotypes and demands greater public education to dispel myths and facilitate comprehensive healthcare strategies. Hansen’s disease is curable – getting an early diagnosis and prompt treatment can help prevent disabilities down the line.
References
https://doi.org/10.1186/s41702-017-0012-5
https://www.cell.com/fulltext/S0960-9822(01)00213-5#secd22632723e174
https://www.who.int/news-room/fact-sheets/detail/leprosy
https://www.frontiersin.org/articles/10.3389/fmed.2022.879097/full
https://www.tandfonline.com/doi/full/10.1080/08830185.2020.1851370
https://onlinelibrary.wiley.com/doi/full/10.1111/imr.12966
https://journals.plos.org/Plospathogens/article?id=10.1371/journal.ppat.1009972
https://journals.plos.org/Plospathogens/article?id=10.1371/journal.ppat.1009972#abstract0